Denial Management Services With Fine Claim-
Denial management is a critical aspect of revenue cycle management in healthcare, and Fine Claim specializes in providing comprehensive solutions to tackle this challenge head-on. In this guide, we’ll explore the intricacies of denial management and how Fine Claim’s expertise can optimize this process for healthcare providers.
The Importance of Effective Denial Management-
Effective denial management is crucial for healthcare providers to maintain financial stability and operational efficiency. By identifying, addressing, and preventing denials, providers can streamline their revenue cycle, minimize revenue leakage, and enhance cash flow.
Benefits of Fine Claim’s Denial Management Service
Partnering with Fine Claim for denial management offers
numerous benefits for healthcare providers.
Benefits of Fine Claim’s Denial Management Service
Partnering with Fine Claim for denial management offers numerous benefits for healthcare providers.
- Maximized Revenue: By reducing denials and accelerating reimbursement cycles, providers can maximize their revenue potential and financial performance.
- Enhanced Efficiency: Fine Claim’s streamlined processes and proactive approach to denial management help improve operational efficiency and staff productivity.
- Improved Cash Flow: Timely resolution of denials ensures a steady cash flow, enabling providers to meet financial obligations and invest in growth initiatives.
- Compliance Assurance: Fine Claim ensures compliance with regulatory requirements and payer guidelines, mitigating risks associated with non-compliance and audit exposure.
- Focus on Patient Care: By entrusting denial management to Fine Claim, healthcare providers can redirect their focus and resources toward delivering high-quality patient care and clinical outcome.
What is denial management in healthcare?
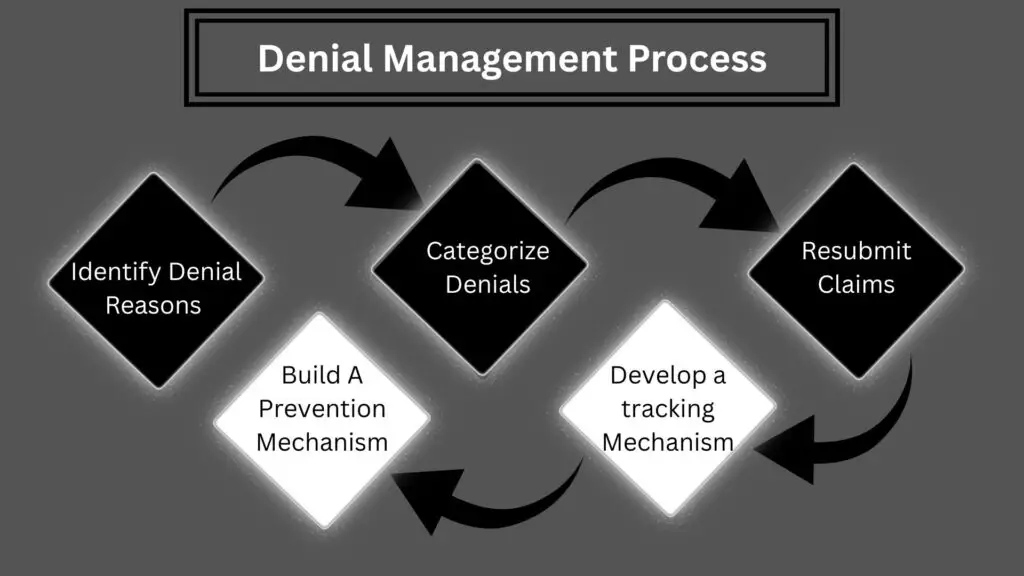
Denial management involves identifying, analyzing, and resolving denied claims from insurance companies to ensure accurate reimbursement for healthcare services provided.
Why do medical claims get denied?
Common reasons include coding errors, missing or invalid patient information, lack of pre-authorization, duplicate billing, timely filing limits exceeded, and non-covered services.
How can we reduce claim denials?
Strategies include accurate patient registration, thorough documentation, regular staff training, and using claim scrubbing tools.
Can denied claims be appealed?
Yes, denied claims can be appealed by providing additional documentation and evidence to support the claim.
What are the benefits of outsourcing denial management?
Outsourcing can reduce administrative burden, improve cash flow, and increase patient satisfaction by leveraging specialized expertise in handling denials.